Nearly131 years ago after the discovery of the Kochs Bacillus, TB even today remains an epidemic out of control in much of the world despite the fact that effective cures which have been made available for decades. The greatest killer of human beings in all history is still at work in spite of many scientific breakthroughs.
Currently, Tuberculosis has become the deadliest infectious disease in the world and the number one infectious killer, causing three (3) millions of deaths per year both youth and adults. This has such serious implications to the world economy, as Tuberculosis kills or disables mainly young people, who form the productive sector of a countries economy, so much so that the World Health Organization (WHO) declared Tuberculosis ‘a global emergency’ in 1993.
Tuberculosis, appearing in many forms that are resistant to multiple drugs (MDR TB) and cannot be cured by once effective medicines together with its deadly partner, the human immunodeficiency virus (HIV), has emerged as one of the most potent threats to mankind and the biggest threat to the world economy.
Why cannot tuberculosis be eliminated? Very simply, it is due to the Low priority tuberculosis is being given by health policymakers. In many low to middle-income countries where less than 1 % of the annual health budget is allocated for tuberculosis - unbelievable, but true. Why the silence? Is it because Tuberculosis is something to be swept under the carpet, covered up, and its existence ignored? The tragic predicament due to inadequate funding has led to inefficient tuberculosis control programmes. This has actually led to a worsening of the world tuberculosis situation.
This is because the patients are not completely cured but do not die of the disease either, leading to a pool of inadequately or improperly treated patients disseminating multi-drug resistant tuberculosis to the community. In other words, in a poor tuberculosis control programme, many patients will eventually die of the disease, true, but there will also be half treated half dead patients disseminating the disease to healthy people. Also, if there were no tuberculosis drugs at all in a country, there would be no multi-drug resistant tuberculosis for it is the improper use of anti-tuberculosis drugs that creates multi-drug resistant tuberculosis. In other words, multi-drug resistant tuberculosis is an entirely man-made by medical practitioners. The drug companies and medical practitioners because they may prescribe drugs in the wrong dosage, wrong combination of the drugs, due to ignorance. Patients, because they have not been told the correct dosage or combination because if the patient has to buy the drugs (as happens when the patients consult a physician privately), he or she may buy less than the prescribed number of drugs or take lesser than the prescribed dosage, to make the drugs last longer, due to the lack of money to buy all the drugs for the prescribed period. The drug companies may produce poor quality drugs which may not have the desired effect.
However, all is not that gloomy. It has been shown conclusively in countries poorer than Sri Lanka, such as Nepal and Bangladesh. (with per capita GNP of around the USD 200, compared to a per capita GNP of US$ 840 for Sri Lanka) That more than 90% of Tuberculosis patients can be cured and the emergence of multi-drug resistant tuberculosis controlled if the treatment of tuberculosis patients are completely supervised. In other words, someone (Nurse, Health Volunteer worker, public health worker a relative) supervises the patient taking the drugs.
Tuberculosis patients (or for that matter any patient) have a bad habit of forgetting to take their drugs when, they feel better, by throwing their drugs away. The very efficacy of the modern anti-tuberculosis drug is in a way disadvantages, because patients feel normal too soon, leading them to stop medication or to take it irregularly. Directly supervised treatment circumvents this hurdle and has now been shown to be the only way in which rampant tuberculosis can be controlled.
As Tuberculosis has been declared a global emergency many efforts have been made to find new effective solutions and strategies in service, design and deliver to eliminate this global menace which manifests in various forms.
New tools, drugs and strategies which are being researched and tried out are bringing effective results.
The DOTS Strategy
Represents a major breakthrough in controlling tuberculosis. No other TB control strategy comes close to being as effective and is affordable as DOTS (Directly Observed Treatment short cause).
The advantages to the community by using the DOTS strategy are numerous.
A. Cures the patients
No other TB control strategy has consistently demonstrated such high cure rates. DOTS produces cure rates as high as 95 per cent, even in the poorest of countries. TB programmes not using DOTS often cure only 40 per cent of their patients.
B. Prevents new infections
DOTS stops the TB Bacillus at the Source by curing the infectious patient. A patient who is not cured will infect, on average, 10 to 15 other people every year.
Stop MDR TB
DOTS makes it virtually impossible to cause a patient to develop the incurable forms of TB that are becoming more common. Other treatment strategies are actually causing multidrug-resistant TB and may be doing more harm than good.
Cost effective
A six month supply of medicines for DOTS cost only $ 11 per patient in some parts of the world. This can be less than the price of a few bottles of aspirin. The World Bank has ranked the DOTS strategy as one of the most cost-effective of all health interventions.
Community-based
DOTS have been demonstrated to add as many years of life as currently available protease inhibitors to HIV positive people. Yet, the medicines used for DOTS are far more cost-effective.
Protects the workforce
Nearly 80 percents of those ill with TB are in their most economically productive years of life. These youthful TB patients represent a workforce nearly as large as the number of people employed by the world's 20 biggest international corporations.
Protects international travellers
There is no other feasible way to protect the world's 500 million annual international travellers from TB. The only safeguard is to use DOTS extensively to reduce the number of infectious. TB cases worldwide.
Stimulates economies
The DOTS strategy offers relatively quick payoffs to the economies of developing countries. Studies in India and Thailand have shown that a small investment in the DOTS strategy can save their economies billions of US dollars.
Proven effective
DOTS has been successfully implemented in a wide range of countries including Sri Lanka, India, Tanzania, Guinea, China, Bangladesh, US and Peru. Currently, nearly 70 countries have begun using DOTS and are achieving good results.
Implementation of the “Stop TB Strategy”
The greatly expanded Tuberculosis diagnosis and treatment services and have saved millions of lives. Development of new tools is a major component of the revised global efforts to stop TB. Progress has been made in this area. They are now in the evaluation process and will be incorporated into the TB control programme in the near future. New and powerful drugs for the Chemotherapy of Tuberculosis are also being developed and progressively introduced into the treatment regimen.
Systematic Strategy for screening and monitoring high-risk zones
Where the population is concentrated such as,
a) Garment Industries b) Factories c) Prison Institutions d) Rehabilitation Camps e) Elderly People's Institutions f) Orphanages g) Mental Asylums h) Low-income communities residing in congested areas.
Changing of the campaign terminology strategy
In the campaign such terms as TB suspects, defaulters, control, tend to criminalize the patient and are patient unfriendly, Therefore in the control of Tuberculosis, consideration is being given to the use of terms which are more humane and patient-friendly which will make the patient more co-operative.
Greater involvement of NGO's in recruiting and mobilizing volunteers for treatment and supervision will make Tuberculosis programmes efficient compared to other South Asian countries, Sri Lanka is far ahead in terms of quality of life, life expectancy, literacy and maternal mortality. This is a constant source of amazement to developed countries, who wonder how we can maintain such indices comparable to a developed country. The answer is, of course, the standard of literacy and education of the population and the solid health infrastructure and active NGOs.
CNAPT initiatives in Sri Lanka
It has been recorded that in countries poorer than Sri Lanka, such as Nepal and Bangladesh, (with per capita GNP of around $ 200, compared to a per capita GNP of US $840 for Sri Lanka) have successfully managed more than 90% of controlled Tuberculosis treatment.
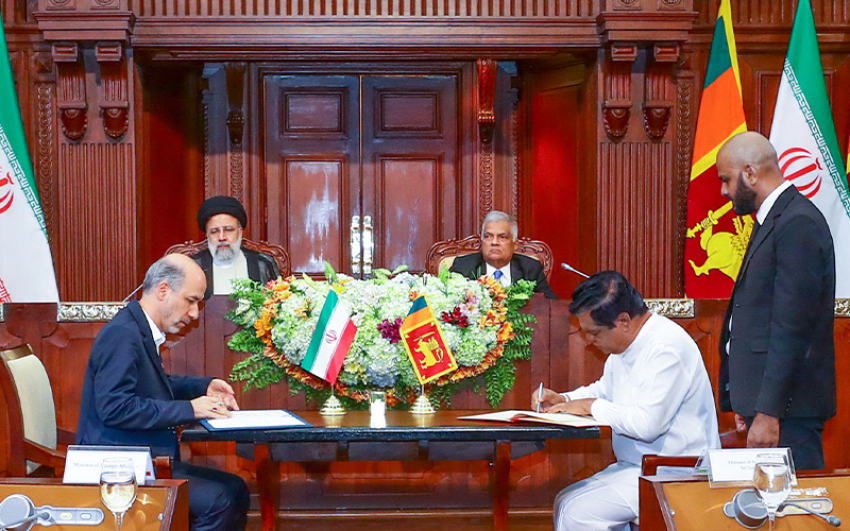
This is where the CNAPT (The Ceylon National Association for the Prevention of Tuberculosis) steps in Educating the public in conducting awareness programmes which are important aspects of TB eradication. The CNAPT has been at the forefront of the campaign for the education of Sri Lankans. Over the last 70 years, the CNAPT has worked in partnership with the Ministry of Health on a diverse range of civil society partners to promote knowledge and understanding of the disease amongst the vulnerable sections of the population thereby improving access to proper medical care.
In 1948 when tuberculosis (TB) was widely prevalent in Sri Lanka, the Ceylon National Association for the Prevention of Tuberculosis (CNAPT) was formed as a Government approved non-governmental organization (NG0), aimed to launch a nationwide TB programme via basic education, programme support and international cooperation. Seventy years ago when medical treatment was at its infancy and TB was rampant with no definitive cure, Dr. J.H.F. Jayasuriya, Chairman of the Rotary Club, Colombo; sponsored a voluntary organisation to combat TB through the auspices of the club. An inaugural meeting was held on June 17, 1948, thus heralding the beginning of the CNAPT.
In 2008 the CNAPT, with financial assistance from the Global Fund for TB and Malaria (GFATM) sponsored a Knowledge, Attitude and Practice (KAP) study, to better understand the gaps in education and the lapses in public behaviour that obstruct the national efforts in TB eradication.
This study was undertaken in collaboration with the medical personnel of the Respiratory Disease Control Programme of the Ministry of Health, the Centre for Social Survey and the University of Sri Jayewardenepura.
With the intention of spreading knowledge regarding TB, its prevention and management as well as to inform the public on how and where to get the help and information required, the CNAPT, with the assistance of the Global Fund, also started a Health Education Programme.
The Primary target group of this education campaign were school teachers whose aim was to take advantage of their strategic position and spread the message to their pupils and through them to the society at large.
The international community, WHO, NGOs and the Sri Lankan Government have done a great deal for the prevention, treatment and management of the disease while also educating the public. Help is available but people need to be informed where assistance and information are available.
People need assistance and when we extend a hand many will willingly grasp it. The CNAPT aims to promote the concept of extending a helping hand by seeking community, public and volunteer assistance. Tomorrow will be better only through our efforts.
Despite their achievements, many TB patients remain undiagnosed. Escalated community involvement coupled with the harnessing of related elements could be the answer to combating this lethal disease and the CNAPT is committed to being a forerunner in fulfilling this goal.
Emphasis on research and development to improve knowledge and skills for diagnosis, treatment and prevention, plus expansion of existing methods may facilitate CNAPT's goals. The Association has striven to educate all facets to the public through technical publications, workshops and seminars. This is how we attempt to combat TB.
TB in children
Special hospital facilities were non-existent for children afflicted by TB. The CNAPT remedied this by constructing three children's wards: Welisara Children's Ward (1952) Hawke Memorial Ward, Kandana (1955) and Clarence Nathnielz Memorial Ward, Welisara (1960) which provided a total of 165 beds exclusively for children. The total cost of Rs. 900,000 was raised through the efforts of the CNAPT.
Since its inception, the Association has concentrated heavily on health education. The objective of the programme was to convey to the public that TB could be cured, patients must take prescribed treatment and those with suggestive symptoms be screened for they must take prescribed treatment. The programme also included lectures to specifically targeted groups, talks via electronic media, participation at public exhibitions and the distribution of TB related literature. The appointment of permanent health educators furthered this cause.
The proximity of the Health Education Centre to the Colombo Museum makes it accessible to any visitors to the Museum who wish to visit CNAPT's Health Education Centre.
Due to the rapid advancement of TB medical treatment, many functions of the CNAPT have been made redundant and today the Association concentrates primarily on promoting health education. The reduction of the duration of treatment from 4 years to 6 months has made it easier for patients to carry on with their everyday routines with the least amount of inconvenience and the stigma attached to TB has all but disappeared.