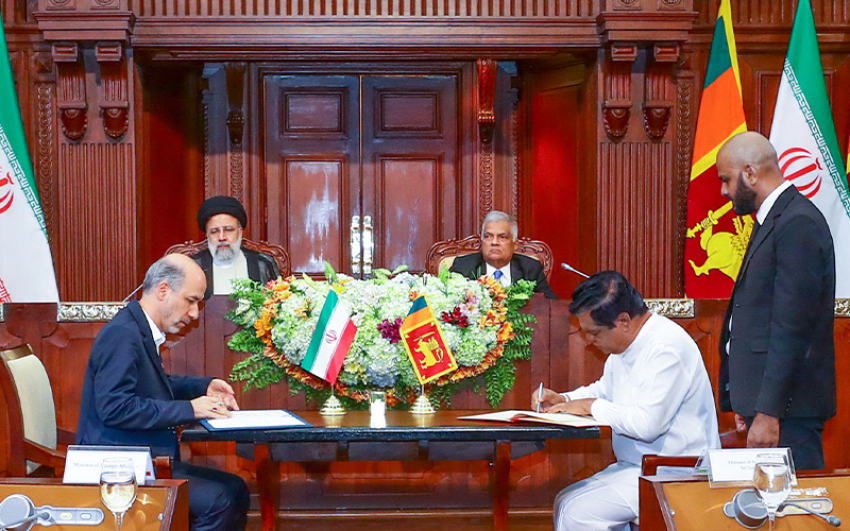
‘Operation Containment’ worked with military-precision. Fanning out for a two-mile radius in rough and rugged terrain in remote Madu Gama, Siyambalanduwa in the Moneragala district, the operation was all about vanquishing a parasite and eliminating the mosquitoes which may be carrying it.
It was a war launched about a year ago by all those who are part of the Moneragala district’s Anti-Malaria Campaign (AMC) in response to the first ‘introduced’ case of malaria after Sri Lanka was declared malaria-free in September 2016, the Sunday Times learns.
Within a week, having drawn up a detailed map with all homes in the area included, the teams had waded across Heda Oya and Meeyan-ara or walked through a uk-kele (sugar-cane jungle) to screen men, women and children for malaria.
The simple but important message for Sri Lanka through this experience is that the spectre of malaria is ever-present, reiterate many experts, pointing out that even though the country has eliminated malaria, vigilance and prompt action are the ‘sentinels’ that should not be dismantled if “we are to maintain and sustain this status”.
“We must never forget the lessons of the past and never let our guard down,” says the Director of the AMC, Dr. Hemantha Herath giving the backdrop in which Sri Lanka was declared malaria-free by the World Health Organization (WHO).
The last case of ‘local’ transmission of malaria in Sri Lanka was reported in October 2012 and the country was under strict review by the WHO, before being declared malaria-free in September 2016, three years ago.
Sri Lanka has eliminated this mosquito-borne disease but the world is yet to do so, warns Dr. Herath, explaining that to maintain malaria-free status until such time as the world eradicates it, which could be in 30-40 years or more, it is essential to maintain at maximum level the skills and expertise of those who have been part of such elimination. There should also be adequate numbers fully oriented towards this cause and resources including infrastructure, equipment and vehicles.
Dr. Hemantha Herath
Every year, we have about 50 ‘imported’ cases of malaria among locals who have travelled out of the country and brought back the disease and foreigners who bring it in. As such, it is essential to detect and treat them as well as do follow-up action, he says, adding that each and everyone – from policymakers to officials, from medical personnel to the public – needs to know the “gravity” of a revival of malaria in the country.
Dr. Herath warns that one local case may not be that tangible but the country cannot be complacent awaiting a flood of cases because by that time it will be too late. We cannot forget 1963, when Sri Lanka “virtually” got rid of malaria, reporting only 17 cases. We thought the war was won and disbanded the AMC and all its numerous activities. What happened? In three to four years, it came back in all its virulence in epidemic proportions, catching in its vice-like grip around 100,000 people in a year.
“Why should we invest to continue to keep Sri Lanka malaria-free,” he asks, with the quick response that malaria is not only deadly but also devastating and has major adverse impacts on socio-economic and cultural life. Of the total health budget of about Rs. 200 billion per year, the AMC is allocated Rs. 1 billion which is 0.5% and covers all 22 health regions and 2,000 health staff [Regional Malaria Officers, Public Health Inspectors (PHIs), Public Health Field Officers (PHFOs), Public Health Laboratory Technicians (microscopists), entomologists and more], as well as equipment and chemicals.
He adds: “This is to our benefit. Scientific studies have found that every rupee spent on fighting malaria saves the government Rs. 13. This means there is a 13-fold saving.”
Referring to the always-present threat, Dr. Herath says that in December 2016 the urban-mosquito Anopheles stephensi usually found in India was detected in the northern regions of Sri Lanka, the Mannar island and the Jaffna peninsula, later spreading to Vavuniya, Kilinochchi, Mullaitivu and Kalmunai. “We camped in the area and managed to restrict it to Mannar island, Jaffna peninsula and Akkaraipattu.”
Next came the first ‘imported’ case of malaria in Siyambalanduwa in November 2018, followed by the first ‘introduced’ case in December 2018 in Colombo, the local having picked up the illness in Siyambalanduwa, he says, going into detail how they mobilised everyone to battle it and even got the necessary funds on January 1 when the whole country was in holiday-mood. “This is why we need people with the right orientation, across the board from the Health Ministry level through to the provincial, regional, district and ground level, in our war against malaria.”
The extent of screening is massive – around one million people every year to catch the first signs of the disease, with about one million blood films being checked, it is understood.
Moneragala’s Regional Malaria Officer Dr. V.M. Karunasena takes up the tale from there, how in November 2018 when on a hospital visit he was informed that an Indian migrant worker from the area had been treated for a bad cough and cold.
“The following day itself, we went to the sugar-cane plantation where the Indian workers were and screened all 32 there using the Rapid Diagnostic Test and microscopic slides. No one was positive for malaria. Ten days later, an Indian worker had got a fever, sought treatment but returned a few days later for hospital admission. We were informed and took immediate follow-up action including indoor residual spraying to destroy the mosquito and screening all those within a one-km radius.
It was after several days that the first ‘introduced’ case – after malaria-free certification – was diagnosed in Colombo in a local. Once again, the action was prompt, the Sunday Times learns, with his case history showing that he had not been abroad where he could have picked up malaria but had been at Siyambalanduwa for a night on work.
This followed intense mapping, hot on the heels of which the spraying, the blood-testing, entomological surveillance and introduction of guppies into wells to destroy the vector and larvicide-spraying in other water bodies to destroy the mosquito larvae, all took place as well as the distribution of bed-nets and awareness programmes.
All these indeed are reality-checks to be extra-vigilant to prevent malaria from coming back in all its ferocity to Sri Lanka.
Through rough and rugged terrain, the Moneragala AMC staff persist to curb and contain malaria in November 2018
Complacency, a big risk
Vigilance and action are what Emeritus Prof. Kamini Mendis also keeps echoing when the Sunday Times meets her recently, while she heaps laurels on the “intense and incredible work” carried out by the Anti-Malaria Campaign (AMC) officials in Siyambalanduwa and Kandy.
Prof. Kamini Mendis
Fervently urging that eliminating malaria should not be the end of vigilance, this malariologist who was attached to the Global Malaria Programme of the World Health Organization (WHO), warns in a timely article published on September 5 in ‘Nature’ – and cited by ‘Science’ – that three years after Sri Lanka was declared free of the deadly disease, “complacency is a big risk”. (The British multi-disciplinary journal of science – ‘Nature’ is reportedly ranked as the world’s most cited journal and one of the world’s top academic journals.)
“I worry that even the medical profession has lost its memory of malaria. Remembering malaria’s devastation is one of Sri Lanka’s biggest challenges in ‘fending’ it off,” says Prof. Mendis, stressing the need to focus on prevention and gaining skills to stop its return. It is vitally important not only to invest funds but also maintain the necessary structures.
Citing a recent scenario, she points out that malaria “surged” back in Venezuela with about a million new cases last year (2018), after the country’s surveillance and health-care systems collapsed.
Next she picks up leprosy from within Sri Lanka, explaining that once the country eliminated leprosy in 1995, the responsibilities of the leprosy campaign were rapidly “bundled” into the national health system. By 2000, the disease had returned, with about 2,000 cases per year.
Prof. Mendis also draws on lessons from history to justify why the country has to expend much effort for a disease that has been eliminated.
“We must not forget that Sri Lanka has a history of a massive epidemic in 1934-35 which saw 80,000 people dying. The maintenance of vigilance is of paramount importance. The cost of this would be minimal compared to what we would have to spend if the disease came back.”
The tight-rope that Sri Lanka walks with regard to malaria becomes obvious when Prof. Mendis says that around September 10, this year, four ‘imported’ cases of malaria were reported from Kandy. The patients were part of a large nade which had gone to India on pilgrimage.
The AMC staff traced every single person, went to their homes and screened them and did the needful.
“All health staff should be constantly reminded about the threat of malaria, while other efforts, such as screening high-risk migrant groups need to be continued. The AMC currently implements programmes through provincial health systems but pressure may mount to integrate malaria surveillance and response into the general health system eventually. The argument is that integrated services are more sustainable than stand-alone ones and that funds dedicated to a disease so rarely seen would be better used elsewhere,” she says, adding that Sri Lanka’s history though warns against taking that step too soon. Keeping this ancient scourge at bay is as important as stamping it out.